Peritoneal Dialysis
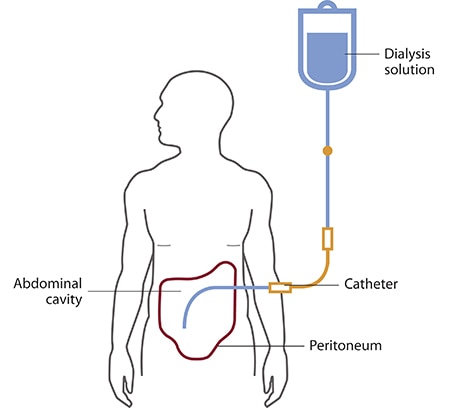
Peritoneal dialysis (PD) is a treatment that uses the lining of your abdomen (belly area), called your peritoneum, and a cleaning solution called dialysate to clean your blood. Dialysate absorbs waste and fluid from your blood, using your peritoneum as a filter. One benefit of PD is that it is not done in a dialysis center. You can do your PD treatment any place that is clean and dry. This can allow you more freedom to work, travel or do other activities you enjoy without worrying about scheduling dialysis appointments. The two most common types of PD are continuous ambulatory PD (CAPD) and continuous cycler-assisted PD (CCPD). Your doctor can help you decide which is right for you.
The benefits of peritoneal dialysis compared with hemodialysis can include:
- Greater lifestyle flexibility and independence. These can be especially important if you work, travel or live far from a hemodialysis center.
- More flexible dietary guidelines. Peritoneal dialysis is done more continuously than hemodialysis, resulting in less accumulation of potassium, sodium and fluid.
- More stable blood chemistry and body hydration. Peritoneal dialysis doesn't require intravenous (IV) access, which can disrupt your circulation and fluid levels.
- Longer lasting residual kidney function. People who use peritoneal dialysis might retain kidney function slightly longer than people who use hemodialysis.
Risks
Complications of peritoneal dialysis can include:
- Infections. An infection of the abdominal lining (peritonitis) is a common complication of peritoneal dialysis. An infection can also develop at the site where the catheter is inserted to carry the cleansing fluid (dialysate) into and out of your abdomen. The risk of infection is greater if the person doing the dialysis isn't adequately trained.
- Weight gain. The dialysate contains sugar (dextrose). Absorbing some of the dialysate might cause you to take in several hundred extra calories a day, leading to weight gain. The extra calories can also cause high blood sugar, especially if you have diabetes.
- Hernia. Holding fluid in your abdomen for long periods may strain your muscles.
- Inadequate dialysis. Peritoneal dialysis can become ineffective after several years. You might need to switch to hemodialysis.
If you have peritoneal dialysis, you'll need to avoid:
- Certain prescription and over-the-counter medications that can damage your kidneys, including nonsteroidal anti-inflammatory drugs.
- Soaking in a bath or hot tub, or swimming in a lake, pond, river or nonchlorinated pool — which increases the risk of infection. Showers and swimming in a chlorinated pool are generally acceptable.
How you prepare
You'll receive training on what peritoneal dialysis involves and how to use the equipment.
You'll also need an operation to insert the catheter that carries the dialysate in and out of your abdomen. The insertion might be done under local or general anesthesia. The tube is usually inserted near your bellybutton.
After the tube is inserted, your doctor will probably recommend waiting at least two weeks before starting peritoneal dialysis treatments to give the catheter site time to heal. Complete healing of the catheter site can take up to two months.
What you can expect
During peritoneal dialysis:
- The dialysate flows into your abdomen and stays there for a prescribed period of time (dwell time) — usually four to six hours
- Dextrose in the dialysate helps filter waste, chemicals and extra fluid in your blood from tiny blood vessels (capillaries) in the lining of your abdominal cavity (peritoneum)
- When the dwell time is over, the solution — along with waste products drawn from your blood — drains into a sterile collection bag
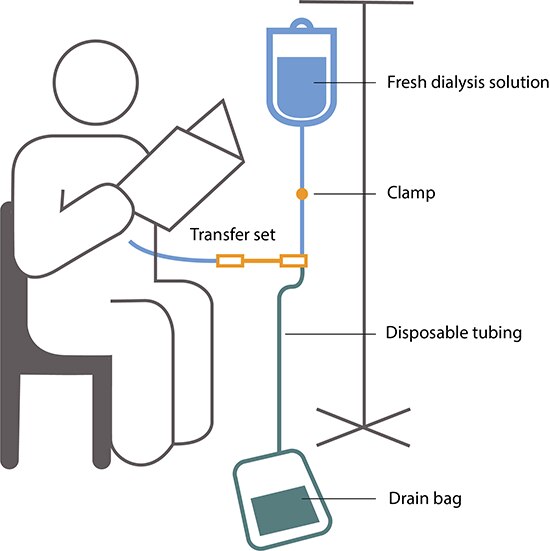
The process of filling and then draining your abdomen is called an exchange. Different methods of peritoneal dialysis have different schedules of exchange. The two main schedules are:
- Continuous ambulatory peritoneal dialysis (CAPD)
- Continuous cycling peritoneal dialysis (CCPD)
Continuous ambulatory peritoneal dialysis (CAPD)
You fill your abdomen with dialysate, let it remain there for a prescribed dwell time, then drain the fluid. Gravity moves the fluid through the catheter and into and out of your abdomen.
With CAPD:
- You may need three to five exchanges during the day and one with a longer dwell time while you sleep
- You can do the exchanges at home, work or any clean place
- You're free to go about your normal activities while the dialysate dwells in your abdomen
Continuous cycling peritoneal dialysis (CCPD)
Also known as automated peritoneal dialysis (APD), this method uses a machine (automated cycler) that performs multiple exchanges at night while you sleep. The cycler automatically fills your abdomen with dialysate, allows it to dwell there and then drains it to a sterile bag that you empty in the morning.
With CCPD:
- You must remain attached to the machine for 10 to 12 hours at night.
- You aren't connected to the machine during the day. But in the morning you begin one exchange with a dwell time that lasts the entire day.
- You might have a lower risk of peritonitis because you connect and disconnect to the dialysis equipment less frequently than you do with CAPD.
To determine the method of exchange that's best for you, your doctor will consider your medical condition, lifestyle and personal preferences. Your doctor might suggest certain modifications to individualize your program.
Results
Many factors affect how well peritoneal dialysis works in removing wastes and extra fluid from your blood. These factors include:
- Your size
- How quickly your peritoneum filters waste
- How much dialysis solution you use
- The number of daily exchanges
- Length of dwell times
- The concentration of sugar in the dialysis solution
To check if your dialysis is removing enough waste products, your doctor is likely to recommend:
- Peritoneal equilibration test (PET). This test compares samples of your blood and your dialysis solution during an exchange. The results indicate whether waste toxins pass quickly or slowly from your blood into the dialysate. That information helps determine whether your dialysis would be improved if the solution stayed in your abdomen for a shorter or longer time.
- Clearance test. A blood sample and a sample of used dialysis solution are analyzed to determine how much of a certain waste product (urea) is being removed from your blood during dialysis. If you still produce urine, your doctor may also take a urine sample to measure its urea concentration.
If the test results show that your dialysis schedule is not removing enough wastes, your doctor might change your dialysis routine to:
- Increase the number of exchanges
- Increase the amount of dialysate you use for each exchange
- Use a dialysate with a higher concentration of dextrose
You can improve your dialysis results and your overall health by eating the right foods, including foods low in sodium and phosphorus. A dietitian can help you develop an individualized meal plan based on your weight; your personal preferences; and your remaining kidney function and other medical conditions, such as diabetes or high blood pressure.
Taking your medications as prescribed also is important for getting the best possible results. While you're receiving peritoneal dialysis, you'll likely need various medications to control your blood pressure, stimulate production of red blood cells, control the levels of certain nutrients in your blood and prevent the buildup of phosphorus in your blood.
- Abdominal hernias in continuous peritoneal dialysis
- Bloody peritoneal dialysate (hemoperitoneum)
- Evaluation of hypervolemia in peritoneal dialysis patients
- Mechanisms of solute clearance and ultrafiltration in peritoneal dialysis
- Microbiology and therapy of peritonitis in continuous peritoneal dialysis
- Modalities for the diagnosis of abdominal and thoracic cavity defects in peritoneal dialysis patients
- Noninfectious complications of continuous peritoneal dialysis
- Noninfectious complications of peritoneal dialysis catheters
- Pathophysiology and prevention of peritonitis in peritoneal dialysis
- Peritoneal dialysis solutions
- Peritoneal equilibration test
- Placement and maintenance of the peritoneal dialysis catheter
- Prescribing and assessing adequate peritoneal dialysis
- Problems with solute clearance and ultrafiltration in continuous peritoneal dialysis
- Rapid transporters on maintenance peritoneal dialysis
- Tunnel and peritoneal catheter exit site infections in continuous peritoneal dialysis
- Urgent-start peritoneal dialysis
- Use of peritoneal dialysis for the treatment of acute kidney injury in adults
Related Conference of Peritoneal Dialysis
14th European Congress on Nephrology, Internal Medicine and Kidney Diseases
Peritoneal Dialysis Conference Speakers
Recommended Sessions
- Acute Renal Failure and Dialysis
- Anemia and Chronic Renal Failure
- Cardiac Disease and Hypertension
- Complications during Dialysis
- Dialysis Adequacy
- Dialysis Modalities
- Endocrine Dysfunction
- Hemodialysis
- Infection and Dialysis
- Intoxications
- Nutrition
- Other
- Peritoneal Dialysis
- Slow Continuous Therapies
- Vascular access
Related Journals
Are you interested in
- Acute & Chronic Kidney Injury: Mechanisms & Early Detection - Nephrologists 2026 (France)
- Acute Kidney Injury - Kidney Care 2026 (UK)
- Acute Kidney Injury (AKI) & Critical Care Nephrology - EURO NEPHROLOGY 2026 (Germany)
- Acute Kidney Injury Mechanisms and Management - UROLOGY 2026 (UAE)
- Aging Populations and Geriatric Epidemiology - EPIDEMIOLOGY-2026 (Netherlands)
- Artificial Intelligence & Digital Nephrology - EURO NEPHROLOGY 2026 (Germany)
- Artificial Intelligence in Nephrology - World Nephrology 2026 (Netherlands)
- Benign Urologic Conditions: Prostate, Bladder & Pelvic Health - Nephrologists 2026 (France)
- Benign Urological Conditions and Management - UROLOGY 2026 (UAE)
- Biomarkers in Kidney Disease - KIDNEY MEET 2026 (UK)
- Biomarkers of Kidney Diseases - Euro Nephrology Summit 2026 (France)
- Biomarkers, Imaging & Diagnostics in Nephrology - EURO NEPHROLOGY 2026 (Germany)
- Cardio-Renal Syndrome - World Nephrology 2026 (Netherlands)
- Cardiorenal Syndrome - Euro Nephrology Summit 2026 (France)
- Cardiovascular Impact of Kidney Disease - KIDNEY MEET 2026 (UK)
- Chronic Kidney Disease - KIDNEY MEET 2026 (UK)
- Chronic Kidney Disease (CKD) – Early Detection & Prevention - EURO NEPHROLOGY 2026 (Germany)
- Chronic Kidney Disease (CKD): Global Epidemiology & Prevention - World Nephrology 2026 (Netherlands)
- Climate Change and Environmental Health - EPIDEMIOLOGY-2026 (Netherlands)
- Clinical Nephrology - Kidney Care 2026 (UK)
- Clinical Nephrology - Euro Nephrology Summit 2026 (France)
- Clinical Trials and Translational Research - UROLOGY 2026 (UAE)
- Critical Care Nephrology - KIDNEY MEET 2026 (UK)
- Diabetic and Hypertensive Kidney Disease - UROLOGY 2026 (UAE)
- Diabetic Kidney Disease & Metabolic Disorders - EURO NEPHROLOGY 2026 (Germany)
- Diabetic Nephropathy - Kidney Care 2026 (UK)
- Diabetic Nephropathy - Euro Nephrology Summit 2026 (France)
- Diabetic Nephropathy - KIDNEY MEET 2026 (UK)
- Diagnostic, Imaging and Radiation Techniques - Euro Nephrology Summit 2026 (France)
- Dialysis - KIDNEY MEET 2026 (UK)
- Dialysis Technologies & Renal Replacement Therapy - EURO NEPHROLOGY 2026 (Germany)
- Diet for Kidney Health - Euro Nephrology Summit 2026 (France)
- Digital Health and Artificial Intelligence Applications - UROLOGY 2026 (UAE)
- Digital Health and Epidemiological Data Science - EPIDEMIOLOGY-2026 (Netherlands)
- Digital Therapeutics, Tele-Nephrology & Remote Patient Management - Nephrologists 2026 (France)
- Drugs for Kidney Diseases - Kidney Care 2026 (UK)
- Drugs used in the treatment of Kidney Diseases - Euro Nephrology Summit 2026 (France)
- Environmental and Occupational Nephrology - World Nephrology 2026 (Netherlands)
- Epidemiology and Global Burden of Renal and Urological Disorders - UROLOGY 2026 (UAE)
- Foundations of Urology and Nephrology - UROLOGY 2026 (UAE)
- Future Directions in Urology and Nephrological Disorders - UROLOGY 2026 (UAE)
- Genetic and Rare Kidney Disorders - World Nephrology 2026 (Netherlands)
- Genetics and Molecular Basis of Kidney and Urological Diseases - UROLOGY 2026 (UAE)
- Genomic Epidemiology and Precision Public Health - EPIDEMIOLOGY-2026 (Netherlands)
- Geriatric Nephrology - Kidney Care 2026 (UK)
- Geriatric Nephrology & Aging Kidneys - EURO NEPHROLOGY 2026 (Germany)
- Geriatric Nephrology: Managing the Aging Kidney - World Nephrology 2026 (Netherlands)
- Geriatric Urology and Renal Health - UROLOGY 2026 (UAE)
- Global Epidemiology and Disease Surveillance - EPIDEMIOLOGY-2026 (Netherlands)
- Glomerular Disease - Euro Nephrology Summit 2026 (France)
- Glomerular Diseases & Autoimmune Nephrology - EURO NEPHROLOGY 2026 (Germany)
- Glomerular Diseases and Management - World Nephrology 2026 (Netherlands)
- Glomerular Diseases, Autoimmunity & Immune Kidney Disorders - Nephrologists 2026 (France)
- Health Systems and Policy Research - EPIDEMIOLOGY-2026 (Netherlands)
- Hematology in Kidney Health - KIDNEY MEET 2026 (UK)
- Hereditary Kidney Disorders - Euro Nephrology Summit 2026 (France)
- Hypertension & Cardio-Renal Syndrome - EURO NEPHROLOGY 2026 (Germany)
- Hypertension & Kidney Health - World Nephrology 2026 (Netherlands)
- Hypertension and Kidney Health - KIDNEY MEET 2026 (UK)
- Hypertension associated with Kidney Diseases - Euro Nephrology Summit 2026 (France)
- Hypertension, Cardiovascular–Renal Axis & Vascular Health - Nephrologists 2026 (France)
- Imaging and Diagnostics in Urology and Nephrology - UROLOGY 2026 (UAE)
- Infection and Immunity in Renal Diseases - World Nephrology 2026 (Netherlands)
- Infectious Diseases and Pandemic Preparedness - EPIDEMIOLOGY-2026 (Netherlands)
- Innovations in Dialysis, Wearable & Implantable Devices - Nephrologists 2026 (France)
- Innovative Dialysis Modalities - World Nephrology 2026 (Netherlands)
- Kidney and Bladder Cancer - Kidney Care 2026 (UK)
- Kidney Diseases & Diagnosis of Kidney Diseases - Kidney Care 2026 (UK)
- Kidney Failure - KIDNEY MEET 2026 (UK)
- Kidney Stones - Euro Nephrology Summit 2026 (France)
- Kidney Stones - KIDNEY MEET 2026 (UK)
- Kidney Transplantation - Kidney Care 2026 (UK)
- Kidney Transplantation - Euro Nephrology Summit 2026 (France)
- Kidney Transplantation - KIDNEY MEET 2026 (UK)
- Kidney Transplantation & Transplant Immunology - EURO NEPHROLOGY 2026 (Germany)
- Kidney Transplantation Science and Practice - UROLOGY 2026 (UAE)
- Kidney Transplantation, Xenotransplantation & Organ Preservation - Nephrologists 2026 (France)
- Kidney Transplantation: Advances & Ethical Considerations - World Nephrology 2026 (Netherlands)
- Lifestyle Factors and Preventive Urology and Nephrology - UROLOGY 2026 (UAE)
- Maternal and Child Health Epidemiology - EPIDEMIOLOGY-2026 (Netherlands)
- Maternal and Child Health Epidemiology - EPIDEMIOLOGY-2026 (Netherlands)
- Mental Health and Behavioral Epidemiology - EPIDEMIOLOGY-2026 (Netherlands)
- Mental Health in Nephrology Patients - World Nephrology 2026 (Netherlands)
- Metabolic Kidney Disorders & Electrolyte Imbalance Management - Nephrologists 2026 (France)
- Migration, Displacement, and Global Health - EPIDEMIOLOGY-2026 (Netherlands)
- Mineral and Bone Disorders in CKD - KIDNEY MEET 2026 (UK)
- Minimally Invasive and Robotic Urological Surgery - UROLOGY 2026 (UAE)
- Minimally Invasive Urologic Surgery & Robotic Innovations - Nephrologists 2026 (France)
- Nephrology - Kidney Care 2026 (UK)
- Nephrology - Euro Nephrology Summit 2026 (France)
- Nephrology Nursing - Kidney Care 2026 (UK)
- Nephrology Nursing - KIDNEY MEET 2026 (UK)
- Nephrology Nursing and Allied Health Roles - World Nephrology 2026 (Netherlands)
- Nephrotic Syndrome - Euro Nephrology Summit 2026 (France)
- Non-Communicable Diseases: Prevention and Control - EPIDEMIOLOGY-2026 (Netherlands)
- Nutrition and Lifestyle in Kidney Health - World Nephrology 2026 (Netherlands)
- Nutrition and Public Health - EPIDEMIOLOGY-2026 (Netherlands)
- Occupational and Industrial Epidemiology - EPIDEMIOLOGY-2026 (Netherlands)
- Pathophysiology of Chronic Kidney Disease - UROLOGY 2026 (UAE)
- Patient-Centered Care and Advocacy - World Nephrology 2026 (Netherlands)
- Patient-Centered Care, Quality of Life & Ethics - EURO NEPHROLOGY 2026 (Germany)
- Pediatric and Geriatric Nephrology - KIDNEY MEET 2026 (UK)
- Pediatric Nephrology - Kidney Care 2026 (UK)
- Pediatric Nephrology - Euro Nephrology Summit 2026 (France)
- Pediatric Nephrology & Congenital Kidney Diseases - EURO NEPHROLOGY 2026 (Germany)
- Pediatric Nephrology & Rare Renal Genetic Disorders - Nephrologists 2026 (France)
- Pediatric Nephrology: Growing Concerns in Children - World Nephrology 2026 (Netherlands)
- Pediatric Urology and Nephrology - UROLOGY 2026 (UAE)
- Pharmacological Approaches in Kidney Disease - KIDNEY MEET 2026 (UK)
- Precision and Personalized Medicine in Renal and Urological Care - UROLOGY 2026 (UAE)
- Precision Medicine & Genetic Kidney Disorders - EURO NEPHROLOGY 2026 (Germany)
- Precision Medicine in Kidney Care - World Nephrology 2026 (Netherlands)
- Public Health Preparedness and Emergency Response - EPIDEMIOLOGY-2026 (Netherlands)
- Public Health, Epidemiology & Global Kidney Care - EURO NEPHROLOGY 2026 (Germany)
- Regenerative Kidney Therapies & Cellular Repair Technologies - Nephrologists 2026 (France)
- Regenerative Medicine and Stem Cell Therapies - World Nephrology 2026 (Netherlands)
- Renal Nutrition - KIDNEY MEET 2026 (UK)
- Renal Nutrition and Metabolism - Kidney Care 2026 (UK)
- Renal Nutrition, Lifestyle & Preventive Care - EURO NEPHROLOGY 2026 (Germany)
- Renal Pathology & Immunology - Kidney Care 2026 (UK)
- Renal Pathology and Immunology - KIDNEY MEET 2026 (UK)
- Renal Precision Medicine & Genomic Risk Profiling - Nephrologists 2026 (France)
- Renal Replacement Therapy and Dialysis Innovations - UROLOGY 2026 (UAE)
- Robotic Kidney Transplantation - KIDNEY MEET 2026 (UK)
- Robotic Surgery - Kidney Care 2026 (UK)
- Smart Nephro-Diagnostics & AI-Enabled Kidney Monitoring - Nephrologists 2026 (France)
- Social Determinants of Health and Health Equity - EPIDEMIOLOGY-2026 (Netherlands)
- Stages of Kidney Diseases - Euro Nephrology Summit 2026 (France)
- Stem cells in Renal Disorders - Euro Nephrology Summit 2026 (France)
- Stem Cells in Renal Disorders - KIDNEY MEET 2026 (UK)
- Technological Advancements in Nephrology - Euro Nephrology Summit 2026 (France)
- The End Stage Renal Diseases & Chronic Kidney Diseases - Kidney Care 2026 (UK)
- Urinary Microbiome, Infection Dynamics & Host Defense - Nephrologists 2026 (France)
- Urinary Tract Infections and Inflammatory Disorders - UROLOGY 2026 (UAE)
- Urologic Oncology: Targeted Therapies & Biomarker Breakthroughs - Nephrologists 2026 (France)
- Urological Oncology Advances - UROLOGY 2026 (UAE)
- Urology - KIDNEY MEET 2026 (UK)
- Urology / Urinary Tract Infections - Kidney Care 2026 (UK)
- Women’s Health and Pregnancy - KIDNEY MEET 2026 (UK)
